Share
Physicians’ Notes: Basic Principles on Medical Death Certification
Go back to MessengerBy Dr. Enrico Risso,
Forensic Pathologist, Deputy Chief Medical Examiner
Physicians perform the final act of care for a patient and their family by completing the medical portion of the death certificate, providing a service for the larger community. The death certificate is a legal document required for burial or cremation of the body, and it must be completed within 48 hours of death. The death certificate is a crucial document for disease surveillance and future planning.
Physicians must be familiar with federal and provincial regulations on medical certifications for death without medical attendance, or unnatural deaths that may require the physician to report the case to the Medical Examiner. Deaths that should be reported to the Medical Examiner are listed on the back page of every death certificate.
If completed properly, a death certificate will communicate the same essential information as a case history. If the cause of death is not properly certified, the document may be ambiguous and the physician may be required to amend the death certificate or provide additional information.
When completing a death certificate, the physician should use the correct death certification form designated by the province and write the cause of death in a legible way, avoiding abbreviations and acronyms (e.g., ACVD, HTN, DM, CVA etc.).
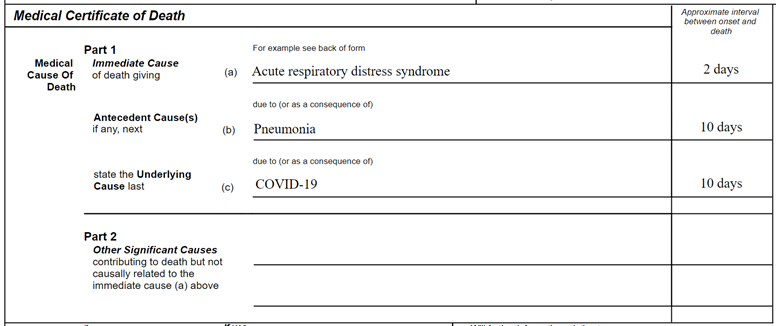
The generic format of a death certificate in Alberta consists of two major parts: respectively named Part I, normally divided in three different lines (a, b and c) that should be filled from top to bottom, completing lines as needed, and Part II.
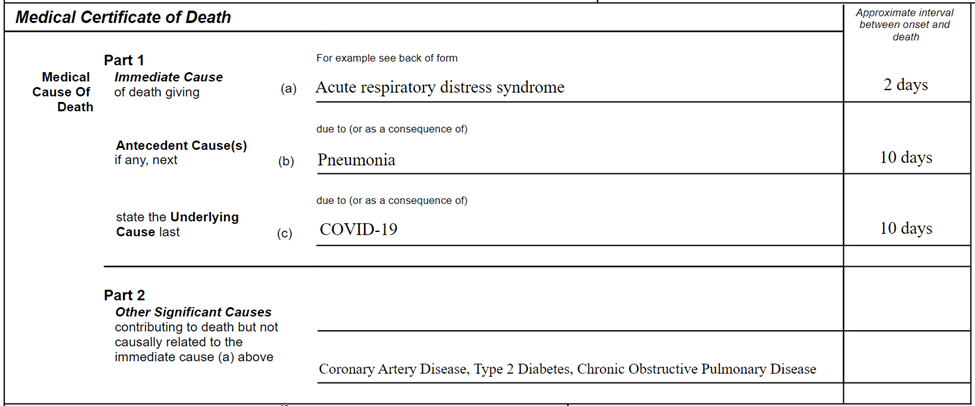
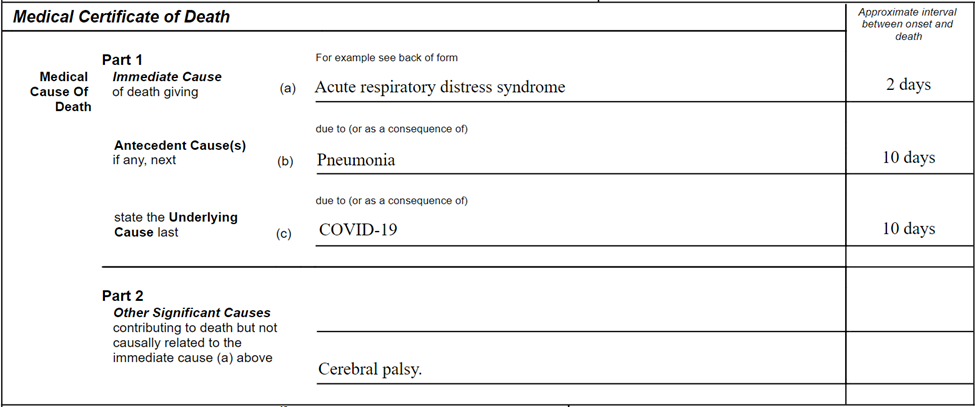
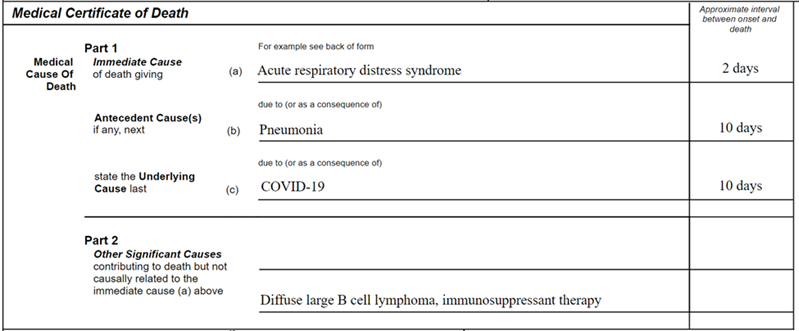
Part I refers to the primary and immediate cause of death, that is to say the underlying disease (condition) that initiated the chain of morbid events leading to death. Part II refers to the conditions contributing to death but not resulting in the underlying cause of death stated above, and should not be used as a repository of conditions that contributed to the cause of death.
After the World Health Organization (WHO) declared COVID-19 a pandemic with increasing mortality, the importance of correctly certifying COVID-19-related deaths is crucial. In view of the public health importance of this infection, when it is thought to have caused death, or is assumed to have caused or contributed to death, it should be recorded in Part I of the medical cause of death. A specification of the causal sequence leading to death (e.g., acute respiratory distress syndrome, or pneumonia) is also important.
The use of official terminology, as recommended by the WHO (i.e., COVID-19), should be used for all certification of this cause of death.
As there are many types of coronaviruses it is recommended not to use “coronavirus” in place of COVID-19. This will help to reduce uncertainty for coding and monitoring these deaths which may lead to underreporting.
If a definite diagnosis cannot be made, but the circumstances are compelling within a reasonable degree of certainty, it is acceptable to report COVID-19 on a death certificate as “presumed” or “probable.”
On a generic model form, a typical death certification should look as follows:
Patients with pre-existing chronic conditions or a compromised immune system due to physical disability are known to be at higher risk. Therefore, conditions such as chronic bronchitis and emphysema, atherosclerotic coronary artery disease or diabetes mellitus should be listed in Part II as significant contributory factors (see below).























Comments for this post are now closed. If you would like to share your feedback on this topic, please email support@cpsa.ca.