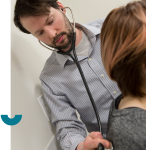
About Physician Assistants
Physician Assistants (PAs) are trained healthcare providers who work under the supervision of a physician. PAs work in a variety of clinical team settings to complement existing services and help improve patient access to quality health care.
PA Regulation
On April 1, 2021, PAs came under CPSA regulation. We’ve supported this move for years and welcome them as the newest regulated member of Alberta’s healthcare team.
As professionals supervised by physicians, PAs are to follow all CPSA Standards of Practice and comply with our continuing competence requirements.
History of PAs
Physician assistants have a long history serving Canadians either in the public healthcare system or in the Canadian Armed Forces. While this may be the first time many have heard of PAs, they’ve played an important role in health care for decades.
"Physician assistants have played an important role in health care for decades."
- Dr. Scott McLeod, CPSA Registrar
Physician Assistant FAQs
All FAQsAs a CPSA registered physician assistant (PA), can I bill Alberta Health for my services?
No. Physician assistants cannot bill Alberta Health independently. PAs are paid by their group or Primary Care Network (PCN).
Do I have to meet all three subclauses in clause 13 of CPSA’s Virtual Care standard before prescribing virtually?
No. The expectation is that at least one of these situations is met in order to prescribe opioids or other controlled substances.
Do military physician assistants (PAs) have to register with CPSA?
If a PA in the Canadian Armed Forces (CAF) is seeing civilian patients in Alberta, they must register with CPSA.
Does my Alberta patient need to be in Alberta to receive virtual care?
Generally speaking, no. Providing virtual care to a patient while they are temporarily out of the province (e.g., vacation, work, school) is typically considered continuity of care. However, confirmation of liability protection should be obtained for patients who spend a large portion of their time out of the country (e.g., “snow birds” who are in the USA for months at a time).
How can I hire a physician assistant?
The Canadian Association of Physician Assistants (CAPA) posts physician assistant (PA) positions on their website free of charge for employers. CAPA can also email job advertisements to their Canada-wide membership (~700 PAs) for a fee of $250. See more information.
How do I bill for virtual care provided to a patient who lives in another province?
Billing is not within CPSA’s purview. For more information, please contact the Alberta Health Care Insurance Plan or the Alberta Medical Association. Inquiries could also be made to the health authority in the patient’s province.
I facilitate virtual care in group settings (e.g., mental health group counselling), do I have to be able to see patients in-person?
If patients cannot be seen in person, the expectation is that the physician would arrange in-person care in a timeframe appropriate for the urgency of the matter. Arrangements would need to be made with the next most appropriate healthcare provider/service to have the person assessed in person (e.g., confirming with the referring healthcare provider that they will see the patient in person if necessary and ensuring the patient understands this arrangement).
I provide services virtually to patients who live in other provinces, do I have to get licences in all of those provinces?
Each province’s College of Physicians & Surgeons has different virtual care/licensure requirements. Physicians are required to confirm with each province what the expectations are and comply accordingly.
I provide virtual care that involves prescribing medications to patients in remote areas where I have not examined the patient and don’t have a pre-existing longitudinal treating relationship (e.g., treatment of substance use disorder requiring OAT, long-acting stimulants, antiviral medication, etc.), do I have to stop this service?
Not necessarily. As long as follow-up care will be arranged or provided going forward, an urgent assessment for/induction of Schedule 1 or 2 drugs would generally meet the criteria for a longitudinal relationship. It is understood that management of this nature is not a one-time interaction without follow-up.
I provide virtual care through a healthcare app, do I have to stop if I can’t provide in-person care to every patient I see virtually?
No. We understand there are times when this is not feasible (e.g., patient lives in a remote location). The expectation is that the physician would arrange in-person care in a timeframe appropriate for the urgency of the matter. This might look like reaching out to the patient’s primary care provider or, if the patient does not have one, contacting local urgent care/emergency department to provide appropriate background information.
My Alberta patient has moved to another province, but wants to continue seeing me virtually, can I do this?
Each province’s College of Physicians & Surgeons has different virtual care/licensure requirements. The requirements of the college in the patient’s new province would need to be determined and followed. Additionally, arrangements would need to be made for the patient to be seen in-person when necessary.
What if I’m out of the province/country? Can I still provide virtual care to Alberta patients?
As long as in-person care can be arranged when necessary, this is acceptable; however, confirmation of liability protection should be obtained. The expectation is that the physician would arrange in-person care in a timeframe appropriate for the urgency of the matter.