Share
Decolonizing health care: the role of immigrant health professionals
Back to MessengerRead time: 2 minutes
By Farzana Ali, PhD (C), Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan
Immigrants constitute one in four healthcare workers in Canada1. Immigrant health professionals play a crucial role in decolonizing healthcare by diversifying perspectives, advocating for culturally competent care, and challenging systemic biases entrenched in global health systems. Their experiences of migration, marginalization, and transnational knowledge enable them to recognize blind spots within Western biomedical paradigms and promote pluralistic approaches to health and healing.
Western medicine in Canada has historically marginalized Indigenous healing through systemic exclusion, regulatory restrictions, and cultural bias. Rooted in colonial ideologies, the healthcare system often dismisses Indigenous knowledge as unscientific despite its longstanding efficacy. This exclusion fosters mistrust and worsens health outcomes for Indigenous peoples.
Immigrant Healthcare Providers as Allies
The Truth and Reconciliation Commission of Canada2 emphasizes that healthcare professionals, including immigrants, must acknowledge, respect, and integrate Indigenous healing into culturally responsive care. Translating this mandate into equitable policies remains challenging. Immigrant providers can serve as vital allies by advocating for culturally safe care, supporting decolonization, and challenging systemic inequities within institutions.
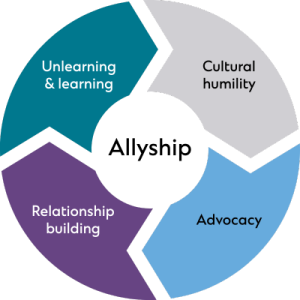 |
Cultural Humility instead of cultural competency
Many health institutions emphasize cultural competence—the idea that providers can master fixed knowledge about cultures—but this often fails in Indigenous contexts where lived histories and spiritual practices resist generalization. Cultural humility, a lifelong practice of self-reflection, listening, and power-sharing, is increasingly recognized as essential for building trust with Indigenous patients. Immigrant healthcare providers, shaped by experiences of cultural dislocation, racialization, and marginalization, may be especially aware of the limits of a competence-based model and better equipped to engage with humility and openness3.
Advocacy in Action: Voices for equity
Advocating for the inclusion of Indigenous healing practices requires more than symbolic recognition—it demands structural integration within the healthcare systems. Immigrant providers, having faced marginalization, can identify systemic imbalances and support Indigenous-led models without overshadowing them. Research shows they are more likely to work in underserved areas and exhibit empathy in cross-cultural care ⁴⁻⁵. In leadership roles, they can leverage their institutional influence to promote reforms, such as integrating Elders into care teams, supporting access to traditional medicines, and securing funding for culturally safe healing spaces.
Bridging worlds: Fostering trust through meaningful relationships
Immigrant providers may relate to colonialism and marginalization, but Indigenous peoples face a unique settler-colonial system of land dispossession and systemic racism2. Unlike immigrants, Indigenous peoples were forcibly displaced within their own lands. Acknowledging this difference fosters more respectful engagement. Adopting a “listen more, speak less”6 approach enables immigrant healthcare providers to build respectful, trusting relationships with Indigenous patients by prioritizing their voices and cultural knowledge. By listening deeply and resisting the urge to lead or correct, providers demonstrate respect, build rapport, and support culturally safe care rooted in Indigenous values and communication styles.
Commitment to ongoing learning and allyship training
Immigrant healthcare providers in Canada must commit to ongoing learning and allyship training to effectively support Indigenous patients and contribute to decolonizing healthcare. This includes deepening knowledge of Indigenous histories and colonial impacts. By engaging in formal allyship training, providers develop the skills to recognize systemic inequities, challenge biases (both personal and systemic), and amplify Indigenous voices respectfully. Continuous education fosters cultural humility and critical reflection on power, which is essential for building trust, promoting health equity, and delivering culturally safe care.
Immigrant healthcare providers bring unique perspectives crucial for advancing equitable and culturally safe care for Indigenous communities. Their role as allies involves not only delivering care but actively challenging systemic barriers and fostering respectful partnerships grounded in understanding and humility. Sustained commitment can reshape healthcare to honour Indigenous knowledge and promote true reconciliation.
 |
Farzana Ali is a doctoral researcher in Community Health and Epidemiology at the College of Medicine, University of Saskatchewan. As a first-generation immigrant woman, her research is deeply rooted in the decolonization of public health and the advancement of patient-centered approaches—particularly for individuals from vulnerable and marginalized backgrounds.
With over nine years of experience in community-based participatory knowledge mobilization, Farzana has worked closely with people living with or affected by HIV and substance use. Her overarching goal is to become a community-engaged scholar, dedicated to facilitating and supporting impactful health research that leads to tangible, measurable improvements in communities. |
References:
- Government of Canada. Growing Canada’s future through immigration: Strengthening the health sector [Internet]. Ottawa (ON): Immigration, Refugees and Citizenship Canada; 2024 [cited 2025 May 18]. Available from: https://www.canada.ca/en/immigration-refugees-citizenship/campaigns/immigration-matters/growing-canada-future/health.html
- Truth and Reconciliation Commission of Canada. Truth and Reconciliation Commission of Canada: Calls to Action [Internet]. Winnipeg, MB: TRC; 2015 [cited 2025 May 19]. Available from: https://ehprnh2mwo3.exactdn.com/wp-content/uploads/2021/01/Calls_to_Action_English2.pdf
- Ali F. Integrating Indigenous knowledge in practice and research: a new way forward for the immigrant health professionals and researchers. In: Reconciliation in Practice: Cross-Cultural Perspectives. October 2019.
- Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Aff (Millwood). 2000;19(4):76–83.
- Saha S, Shipman SA. Race-neutral versus race-conscious workforce policy to improve access to care. Health Aff (Millwood). 2006;25(2):417–29.
- Browne AJ, Varcoe C, Lavoie J, Smye V, Wong S, Krause M, et al. Closing the health equity gap: evidence-based strategies for primary health care organizations. Int J Equity Health. 2012;11:59. doi:10.1186/1475-9276-11-59.
Related News
All News & EventsJune 19, 2025
Innovative collaboration to support Indigenous and rural health care
June 19, 2025
From Treaty obligations to medical curriculum: embedding Indigenous health in physician training
June 19, 2025
Decolonizing health care: the role of immigrant health professionals
June 19, 2025





















Comments for this post are now closed. If you would like to share your feedback on this topic, please email support@cpsa.ca.