About the CPSA Healthier Albertan Grant
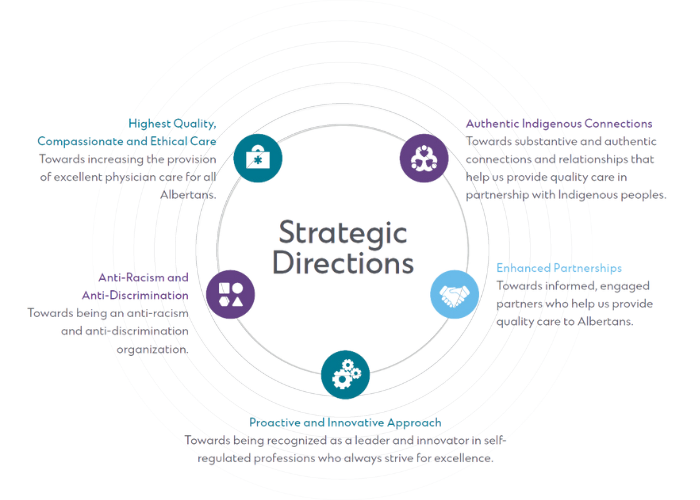
As a learning organization, CPSA is committed to finding new and innovative approaches to ensure Albertans receive safe, high-quality care. This is why we created the CPSA Healthier Albertan Grant. It is a one-time grant program to support Alberta-based organizations and/or individuals with their projects, initiatives and/or research that align with at least one of CPSA’s strategic directions and will directly benefit the health of Albertans or improve their care.
The submission process closed on Feb. 28, 2023 and the CPSA Healthier Albertan Grant recipients are listed below.
Benefitting Albertans
The ultimate goal of the CPSA Healthier Albertan Grant is to benefit the health of Albertans or improve their care. CPSA received over 150 high-quality proposals from organizations and individuals across the province working collaboratively to improve the healthcare experiences of Albertans. The Evaluation Committee looked over each proposed initiative, first without and then with identifying information, and took various factors into account including alignment with CPSA’s strategic directions, feasibility, impact potential and available funding resources.
CPSA Healthier Albertan Grant Recipients
CPSA thanks all applicants for their valuable submissions and is thrilled to announce the 10 impactful initiatives that have been selected for the CPSA Healthier Albertan Grant.
Based on the scope of their projects, applicants had the opportunity to choose the amount awarded based on the following categories when submitting their application form.
Amount awarded categories:
Small Grant – $50,000 – $100,000
Medium Grant – $100,001 – $1,000,000
Large Grant – $1,000,001 – $2,500,000
Supporting Patients by Family Education in Psychotic Illness: A Longitudinal Pre-Post Study
Description by the recipient(s): A lack of resources for family carers of young adults with psychotic illnesses leaves a service gap in early intervention strategy. Public health systems gain an invaluable ally by educating and supporting family carers. The primary research goal is to implement a psychoeducational intervention for family carers, created and delivered collaboratively by healthcare professionals and individuals with lived experience to reduce family burden and foster community stabilization of the young adults. The pilot study showed feasibility of course implementation, identified delivery barriers, and gathered qualitative and longitudinal quantitative data from participants. The Phase II study is underway which evaluates long term outcomes (two years post intervention) in 111 family carers and where possible, their matched young adults with psychosis. Family carers of young adults aged 17-27 who had recent psychosis related hospital admissions in Edmonton Zone are eligible to enrol. Nine evidence-based, expert-reviewed and family peer-informed psychoeducational modules are delivered by video conferencing in two-hour sessions over nine weeks to family carers. The modules combine education about psychosis with LEAP© skills (Listen, Empathize, Agree, Partner) and ACT (Acceptance and Commitment Therapy). A major deliverable of the overall study is to produce a standardized facilitators’ manual for widespread dissemination and uptake in the public health care system.
Albertans Impacted: 100 Edmonton families with young adults experiencing mental illness with plan to expand to 120 additional families in the future
Organization(s)/Individual(s): Dr. Melanie Robles (Family Medicine), Dr. Adam Abba-Aji (Psychiatry) and Katherine Shettell (Social Worker)
Amount awarded: Small
POWER Program: Personalized Osteoporosis Care With Early Recognition, A Novel Digital Provincial Outpatient Fracture Liaison Service
Description by the recipient(s): At least one in three females and one in five males will experience a fragility fracture (FF) due to osteoporosis or low bone mass in their lifetime. Individuals who experience a FF are two to four times more likely to have another fracture in the future. FFs result in decreased functional independence, increased admission to long-term care centres and significant mortality rates. Patients with FF have low rates of osteoporosis investigation and treatment initiation. Therefore, without early identification, investigation and intervention (3i model of care), the incidence of FF will continue to increase.
Our novel virtual POWER Program (Personalized Osteoporosis care With Early Recognition) will be the first digital 3i outpatient fracture liaison service (FLS) in Canada. This program employs a centralized, digital multidisciplinary collaborative system designed to decrease the fragmentation of acute FF care, improve equitable access and bridge the osteoporosis care gaps in Alberta. The POWER Program will engage patients at the time of their sentinel fracture to prevent future FF throughout their lifespan. Our digital health solution consists of a smartphone application, program-specific website, and virtual patient and specialist support. A personalized care plan will be initiated to address bone health care gaps and digital follow-ups will occur as needed based on risk stratification. This program aims to improve the sustainability of Alberta’s health system with a solution that will improve quality, accessibility and equity of care, while ultimately saving costs, reducing acute care utilization and preventing Albertans from suffering the morbidity, mortality and loss of independence associated with FF. The POWER Program will support patient engagement in life-long bone health care.
Albertans impacted: All Albertan women over 50 (men over 60) and by extension, younger Albertans who might experience fewer fractures as they age
Organization(s)/Individual(s): Dr. Prism Schneider (University of Calgary)
Amount awarded: Large
Bridge Healing: Access to Transitional Housing from the Emergency Department
Description by the recipient(s): Bridge Healing provides emergency department patients experiencing houselessness with immediate access to transitional housing and a continuum of other health and social supports. It is a partnership between Jasper Place Wellness Centre, the Royal Alexandra Hospital and Alberta Health Services (Edmonton Zone). The primary objective of this research is to determine if patients without housing who access the emergency department can be successfully transitioned to stable housing that meets their needs and budget after referral to the Bridge Healing program. We will also be looking at whether enrolment in Bridge Healing results in a change in the number of emergency department visits, days in hospital and EMS transports that people have in the 6-months before and after enrolment in the program. A community advisory group of individuals who have experienced or are experiencing houselessness will guide all aspects of this work.
Albertans impacted: Vulnerable patients experiencing houselessness
Organization(s)/Individual(s): Dr. Kathryn Dong (University of Alberta)
Amount awarded: Medium
Mind-body In Long Covid and Myalgic Encephalomyelitis Study (MILES): A Patient-Centred RCT
Description by the recipient(s): The Mind-body In Long Covid and Myalgic Encephalomyelitis Study (MILES): A Patient-Centred RCT project will investigate the effectiveness of a mind-body intervention for individuals who meet criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) after COVID-19 infection compared to individuals diagnosed with idiopathic ME/CFS. These complex conditions are post-viral syndromes, sharing similar symptoms and pathophysiology including issues with the central nervous system, immune system, cardiovascular function, metabolism and gut microbiome. Central sensitization (CS), which involves hyper-excitement of central neurons, may worsen symptoms of many chronic conditions including ME/CFS due to Long COVID. To find potential solutions, the research team plans to conduct a multiple-methods wait-list controlled randomized control trial to improve patient-reported outcomes such as health-related quality of life, fatigue, pain and cognitive dysfunction. The study will also investigate metabolomic profiles and microbial signatures in these individuals. Our team firmly acknowledges ME/CFS and Long COVID as serious, debilitating, biomedical conditions. Mind body interventions teach consistent, self-directed use of purposeful thoughts, feelings and actions that support changes in biology and function. If successful, this non-pharmacological intervention could significantly enhance patients’ quality of life and provide valuable insights into managing complex chronic conditions.
Albertans impacted: Albertans who have or will have COVID-19 (estimated 15% developing long-COVID) as well as immigrant, racialized and Indigenous communities due to COVID’s disproportionate affect on these groups
Organization(s)/Individual(s): Co-Principal Investigators (PIs): Dr. Sunita Vohra, MD MSc FRCPC FCAHS, Faculty of Medicine & Dentistry, University of Alberta and Dr. Eleanor Stein, MD FRCPC, Cumming School of Medicine, University of Calgary, Qualitative PI: Dr. Douglas Gross, Ph.D., BScPT, Faculty of Rehabilitation Medicine – Physical Therapy, University of Alberta, Wearable Technology PI: Dr. Victor Ezeugwu, PhD., PT, Faculty of Rehabilitation Medicine – Physical Therapy, University of Alberta, Metabolomics PI: Dr. Jane Shearer, PhD, Department of Biochemistry and Molecular Biology, Cumming School of Medicine, University of Calgary and Microbiome PI: Dr. Christina Thornton MD, PhD, FRCPC, Departments of Medicine, Microbiology, Immunology and Infectious Diseases, Cumming School of Medicine, University of Calgary.
Amount awarded: Medium
Mobile Comprehensive Diabetes Care for Underserved Individuals in Alberta: A Collaboration Between An Academic Institution and a Community Health Centre
Description by the recipient(s): These funds will allow my team to provide full-service diabetes specialty services through a Diabetes Wellness Mobile Clinic (DMC), provided in-kind through the Alex Community Health Centre. This program will be offered within Calgary and surrounding areas, rotating between locations that are designed to be accessible to patients who face social and structural disadvantages. The DMC team will offer diabetes specialist consultations, diabetes education appointments, and screening for macrovascular and microvascular complications to patients who have not been recently screened. Using mobile tools and technologies, patients will undergo all necessary screening right on the bus. Once the need for specific subspecialist care has been identified, the DMC team has developed a specialized referral process to arrange follow-up appointments with much less delay than through standard practices. The team will also invite patients to participate in an evaluation of the program.
Albertans impacted: Adults with diabetes from vulnerable populations (experiencing houselessness, facing financial barriers and Indigenous peoples)
Organization(s)/Individual(s): Dr. David Campbell (University of Calgary) and Emma Wissink, RN (The Alex Community Health Centre)
Amount awarded: Medium
BMSA Health Fair
Description by the recipient(s): The Black Medical Student Association (BMSA) Health Fair is an annual, free event, designed for Edmonton’s Black communities. The goal of this event is threefold:
- Provide a fun, family-friendly, engaging, culturally relevant, and stress-free environment for structurally marginalized Black community members to enjoy activities for all ages
- Organize information booths related to various health and wellness topics relevant to the African, Caribbean, and Black (ACB) community to support education, healthy behaviors, and resource gathering.
- Create a platform for the BMSA to mentor ACB youth about the journey to medicine, being a medical student, and representation within healthcare to aid in intra-community development aiming to increase ACB representation in medical schools.
We have organized booths relevant to the health and educational needs of the Black community including but not limited to nutrition and obesity, family planning, sickle cell disease, 2sLGBTQ+ health, mental health, the Canadian healthcare system for newcomers, youth mentorship, preventative medicine, and more. We’ve partnered with community organizations such as the Africa Centre and community leaders (physicians, social workers, psychologists, and dieticians) to facilitate teaching and education at these booths for our attendees. To encourage participation, the Health Fair is completely free, and people can drop-in when convenient. We will have kid-friendly activities such as a henna artist, face painting, a bouncy castle monitored by volunteers.
In summary, the goal of BMSA’s Health Fair is health education for us, by us. All students involved in the planning are BIPOC, gender-diverse, low socioeconomic status, or refugees. We are passionate about engaging our communities in their health and committed to making this event a success.
Albertans impacted: African, Caribbean, and Black community members
Organization(s)/Individual(s): Black Medical Student Association (BMSA), University of Alberta
Amount awarded: Small
Prevalence and gaps in management of anemia and iron deficiency in reproductive age women in Alberta
Description by the recipient(s): Hemoglobin carries oxygen in the body and is very important. To make hemoglobin, you need iron. Without enough iron, you can have low hemoglobin (anemia). Low iron (iron deficiency) anemia causes many serious symptoms that can affect school, work and daily activities. Iron deficiency anemia is a very common health problem. It is a bigger problem for young women because they lose iron during menstrual periods and pregnancy. About 1 in 10 young women have an iron deficiency. It is very easy to test for iron and hemoglobin levels. There are many simple ways to treat iron deficiency anemia. Despite this, previous Albertan studies have shown that iron deficiency anemia is not diagnosed or treated properly in pregnant women. It is also not clear how other things can affect anemia in young women (i.e. living in a rural place, having a low income, being of different ethnicities including Indigenous or immigrant backgrounds).
We would like to study this topic to try and figure out which young women are at the highest risk of iron deficiency anemia and identify better ways to diagnose and treat this. To answer these questions, we will interview people who are at risk of iron deficiency and healthcare professionals who treat iron deficiency anemia to identify the blocks to understanding and treating anemia. We will use large healthcare databases which record when people go to see doctors or visit the hospital to see how common it is for young women especially in vulnerable groups to get iron deficiency anemia. We hope that the results can help the province make better pathways to find and fix this common problem.
Albertans impacted: All women including those from Indigenous and rural communities and those with a low socioeconomic status
Organization(s)/Individual(s): Drs. Haowei (Linda) Sun and Cynthia Wu (University of Alberta)
Amount awarded: Small
Using real world evidence to evaluate medication safety in pregnancy
Description by the recipient(s): Presently, it is estimated that approximately 60% of pregnant people take medications to manage pre-existing or pregnancy-associated health conditions; however, almost all these medications are taken ‘off-label’, with over 90% of approved medications lacking basic safety data for use during pregnancy. Ultimately, pregnant people (and their physicians) often make difficult decisions regarding medication use in pregnancy without the benefit of data and evidence to help guide their decisions. While randomized controlled trials and detailed pharmacokinetic studies are an ideal way to study medication safety in pregnancy, recruitment into these trials is complex and presently it takes approximately 27 years before there are sufficient published data on new medications to provide even a crude estimate of teratogenic risks in humans. Real-world data generated from existing health care sources can help fill this gap and represent an important, yet under-utilized, tool to assess medication safety in pregnancy. The present study will use real-world data generated from Alberta’s administrative health data holdings, which contain detailed data on medication use along with maternal and infant incomes, to conduct a series of target trials that directly compare the safety of medications used to treat cardiovascular disease in pregnancy to a) non-pharmacologic therapy and b) other medications.
Albertans impacted: Pregnant women, physicians and other allied health professionals
Organization(s)/Individual(s): Dr. Amy Metcalfe (University of Calgary)
Amount awarded: Medium
Improving the quality of the Patient Medical Home for patients: implementing person-centred quality indicators in primary care in Alberta
Description by the recipient(s): This project aims to enhance the quality of the Patient Medical Home in Alberta by implementing Person-Centred Quality Indicators (PC-QIs) in primary care. These indicators, developed collaboratively with patients and healthcare providers, serve as evidence-based tools to ensure person-centred, interdisciplinary care. The research, funded by the CPSA, builds on prior work with primary care partners and aims to co-design the PC-QI implementation, study influencing factors, create supportive materials, and evaluate changes in care quality. The study will initially focus on seven academic clinics before expanding to family practices and Primary Care Networks over a two-year period. Through collaboration with existing partners and a focus on health equity and inclusion, the project strives to provide high-quality, patient-centered care in diverse Alberta populations. The findings will inform the widespread adoption of PC-QIs, ensuring sustained, person-centric care within the Patient Medical Home model while aligning with provincial performance measurement initiatives.
Albertans impacted: 520,000 patients with potential to help all Albertans in the future
Organization(s)/Individual(s): Dr. Maria J. Santana (University of Calgary)
Amount awarded: Medium
An innovative model of equitable cancer care: Indigenous Cancer Patient Multidisciplinary Rounds
Description by the recipient(s): “Indigenous Cancer Patient Multidisciplinary Rounds” is an innovative, whole person, equity promoting model of care, developed in Alberta for Indigenous cancer clients. This project will tell the stories of these rounds and share this model of care. Rounds offer a way to strengthen relationships, catalyse and sustain groups to work together to improve the health not only of Indigenous Albertans, but for the benefit of others facing systemic inequities.
Albertans impacted: Indigenous patients with cancer, Indigenous communities and health workers, and multidisciplinary providers
Organization(s)/Individual(s): Dr. Jessica Simon (University of Calgary)
Amount awarded: Medium
The Evaluation Committee remained independent throughout the selection process. Committee members signed conflict of interest declarations and are under a continuing obligation to make full disclosure to CPSA’s Council Chair of any situations involving actual, perceived or potential conflicts of interest, whenever such situations may arise.
History of the grant funding
From 2012–2016, CPSA collected $150 from each regulated member as part of their annual renewal with the intent to purchase or build a new office space to accommodate CPSA’s growing team. However, with favourable lease rates in 2018, Council decided to continue leasing in downtown Edmonton until at least 2029 and use a portion of CPSA’s Building Fund Reserve towards operations for 2022.
In 2020, Council sought feedback from the profession to help decide what to do with the remaining money that had grown to over $9 million with interest from investments. Ultimately, $4.7 million was used towards operations, thereby creating a one-time annual fee reduction for all practising Alberta physicians in independent practice for 2022, which has been completed. Following that, Council approved allocating $5 million to support programs, initiatives and/or research to benefit Albertans.
In 2022, the CPSA Building Fund Initiatives Working Group presented the recommendation to establish a grant program― the CPSA Healthier Albertan Grant, which Council approved at their Sept. 2022 meeting. The grant launched on Nov. 1, 2022 and final proposals were due Feb. 28, 2023.
Questions?
Email: Grants@cpsa.ab.ca
Phone: 780-969-4983 | 1-800-561-3899 ext. 4983